Hepatitis E: zoonotic emerging disease in industrialized countries
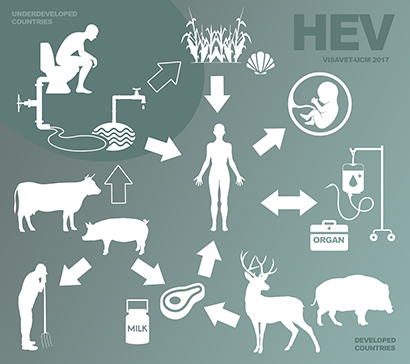
Hepatitis E virus (HEV) is the main cause of viral acute hepatitis in humans worldwide. In endemic areas the virus is mainly transmitted through contaminated water, while in industrialized countries sporadic cases are basically related to animals and hepatitis E is currently considered an emerging zoonotic disease. Besides swine, there are other wild animals such as wild boars and deers which can be reservoirs of this disease. The origin of infection in humans is linked to direct contact with infected animals or to consumption of raw or undercooked meat and liver.
HEV is an RNA virus and therefore it is very difficult to grow it in cell cultures; the majority of diagnostic techniques are aimed to detect the genetic material, but they don´t determine whether the virus is viable (infective) or not. There are 4 major genotypes of HEV. Genotype 3 is the most prevalentin Europe, and it is shared by humans and animals (mainly pigs).
In humans, HEV can cause a bening, acute or self-limiting infection. However, chronic hepatitis E occurs occasionally, mostly associated with inmunocompromised patients, mainly in solid organ transplant ones. Altought the disease usually courses with low mortality (0.2-3%), it could be extremely serious in pregnant women (genotype 1).
Diagnosis is made by serological techniques, mainly ELISAs which detect both IgGs and IgMs and also by using molecular biology techniques, mainly real time PCRs aimed to detect RNA from the virus in different types of samples (feces, blood, liver, etc.) and which are highly sentitive and specific.
There is no effective treatment against hepatitis E. Often the recovery occurs naturally, except in specific occasions in which antivirals, inmunosupressive agents or other drugs are neccesary. Currently there is only one recombinant vaccine approved in China.
From the food security perspective it is relevant that human cases have been associated to pork meat, liver and derivatives (sausages, pâtés, etc.) consumption and, to a lesser extent, from wild animals. Besides, the presence of HEV has been described in molluscs and dairy milk, (even subjected to treatments of pasteurisation) although to date no clinical cases have been reported to be related to dairy products.
Studies in relation to how the different procedures of food (temperature, salt, pH, etc.) affect the survival of HEV in pig products are scarce. HEV is very stable at high temperatures and it can remain viable at a temperature of 56ªC for 1 hour. To inactivate the HEV in pig liver, it is necessary to reach a central temperature of 71 ° C for 20 minutes. However, it is indispensable to perform this type of analyses in other matrices as its composition (eg: fat content) can protect the virus from heat treatment. Freezing does not affect the virus and it has been demonstrated that it remaisn viable after more than 10 years in fecal samples and after several freeze/thaw processes, confirming the stability of the virus. The HEV is also quite resistant to acid pHs.
FAQ
How can humans de infected by Hepatitis E?
Transmission routes are, basically, fecal-oral by contamination of water supplies (most of them in developing countries) and through raw or undercooked contaminated food (most cases in industrialized countries). Cases have also been described by transfusions, transplants and mother-to-child routes.
The vast majority of HEV infections are subclinical and self-limiting. It can cause chronic severe hepatitis in immunocompromised patients, patients with prior liver disease or pregnant women, even to cause fulminant liver failure and cirrhosis.
Who is considere personal at risk?
Personal in contact with pigs and wild animals (veterinarians, salughterhouse staff, swine farmers, hunters, etc.).
Population susceptible from suffering severe diseases: immunocompromised patients, pregnant women, people with previous liver diseases.
Which food can be considered at most risk?
Sausages and products containing liver and blood, mainly. Also meat which has not been properly cooked.
Which thermal treatments are required to ensure the destruction of the virus?
A minimum central temperature of 71 ° C for 20 minutes is required to inactivate the HEV in meat products. Above 80 ° C the inactivation is variable, and is dependent on the amount of virus present in the sample and the heating time. Short heat treatments, even when carried out at high temperaturas, may not be sufficient to inactivate the virus.
Dairy products should be taken into account as the pasteurization does not ensure the destruction of HEV.
Can freezing inactivate the VHE?
Freezing does not affect the viability of the virus.
Which physico-chemical conditions (wa, pH, etc.) affect the survival of the virus?
There are few studies and they have not been standarizated. Most of them have been done in in vitro models. The effect on different products is unknown.
HEV is relatively resistant to acid pH conditions (including pH< 3).
Which recommendations should be done in order to eliminate the risk in cooked meat and offal?
Intense cooking (at least 20 minutes up to 71 ° C) and avoiding cross contamination with other products and materials (blood or contaminated materials such as knives, for example, since the survival of the virus on surfaces and material is demonstrated). Establishing good hygiene practices.
What actions should be implemented into the meat chain to minimize this problem?
The HEV contamination in food may come from the primary production to slaughter and processing steps (through contaminated water used in processing, for example). Therefore, measures should be taken at all stages of the food chain, basically stablishing good hygiene practices. In addition, the HEV awareness campaigns, aimed at the general population and, especially, to the risk groups should be performed.
Research studies are key, because there are many aspects on the epidemiology of the HEV that are unknown, mainly:
- To determine the true HEV prevalence from the farm to the final product by using specific and sensitive diagnostic techniques.
- To establish a optimal cell culture system that allows to obtain large amounts of virus. This is basic to perform pathogenesis studies, to develop vaccines and appropriated diagnostic systems.
- To establish a good experimental animal model in order to carry out infectivity studies and to develop effective vaccines.
- To investigate the survival of the virus in the environment (water, materials, manure, etc.).
- To determine all risk products and the treatments that can inactivate the virus (high pressure, heat treatments, curing, etc.).
Para más información puede dirigirse a:
Neglected and Emerging Diseases Unit
VISAVET Health Surveillance Centre
Complutense University Madrid (Spain)
Tel.: (+34) 913944096
ned@visavet.ucm.es
Bibliography
- Barnaud et al. 2012. Thermal Inactivation of Infectious Hepatitis E Virus in Experimentally Contaminated Food. Appl Environ Microbiol. 78(15):5153-5159.
- Berto et al. 2012. Prevalence and transmission of hepatitis E virus in domestic swine populations in different European countries. BMC Res Not. 5:190.
- Clemente-Casares et al. 2003. Hepatitis E Virus Epidemiology in Industrialized Countries. Emerg Infec Dis. 9(4):449-454.
- Di Bartolo et al. 2012. Hepatitis E Virus in Pork Production Chain in Czech Republic, Italy, and Spain, 2010. Emerg Infec Dis. 18(8).
- Diez-Valcarce et al. 2012. Occurrence of Human Enteric Viruses in Commercial Mussels at Retail Level in Three European Countries. Food Enviro Vir. 4(2):72-80.
- de Deus. Segalés. 2008. Epidemiological study of hepatitis E virus infection in European wild boars (Sus scrofa) in Spain . Vet Micro. 129(1-2):163-170.
- Emerson et al. 2005. Thermal Stability of Hepatitis E Virus. J Infec Dis. 192(5):930-933.
- Feagins et al. 2007. Detection and characterization of infectious Hepatitis E virus from commercial pig livers sold in local grocery stores in the USA. J Gen Vir. 88:912-917.
- Feagins et al. 2008. Inactivation of infectious hepatitis E virus present in commercial pig livers sold in local grocery stores in the United States. Int J Food Microbiol. 123(1-2):32-7.
- Huang et al. 2016. Excretion of infectious hepatitis E virus into milk in cows imposes high risks of zoonosis. Hepatology. 64(2)350-359.
- Intharasongkroh et al. 2016. Hepatitis E Virus in Pork and Variety Meats Sold in Fresh Markets. Food Envir Vir. 9(1):45-53.
- Jimenez de, Oya. 2007. Hepatitis E virus: zoonotic implications. Gastroenterol Hepatol. 30(7):408-18.
- Kukielka et al. 2015. Constant Hepatitis E Virus (HEV) Circulation in Wild Boar and Red Deer in Spain: An Increasing Concern Source of HEV Zoonotic Transmission. Trans Emerg Dis. 63(5):e360-e368.
- Lapa et al. 2015. Epidemiology of Hepatitis E Virus in European Countries. Int J Molec Sci. 16(10):25711-25743.
- Meng et al. 2011. From barnyard to food table: The omnipresence of hepatitis E virus and risk for zoonotic infection and food safety. Vir Res. 161(1):23-30.
- Pavio et al. 2010. Zoonotic hepatitis E: animal reservoirs and emerging risks. Vet Res. 43(6):41:46.
- Renou et al. 2014. Foodborne Transmission of Hepatitis E Virus from Raw Pork Liver Sausage, France. Emerg Infec Dis. 20(11):1945:1947.
- Riveiro-Barciela et al. 2012. Hepatitis E: Dimensión del problema en España. Gastro Hepat. 35(10):719-724.
- Rodríguez-Frias et al. 2012. Hepatitis E: virología molecular, epidemiología y patogénesis. Enf Inf Micro Clin. 30(10):624-634.
- Ruggeri et al. 2013. Zoonotic transmission of hepatitis E virus in industrialized countries. New Micro. 36:331-344.
- Said et al. 2014. Hepatitis E virus in England and Wales: indigenous infection is associated with the consumption of processed pork products. Epidem Infect. 142(7):1467-1475.
- Sridhar et al. 2015. Hepatitis E: A disease of reemerging importance. J Form Med Assoc. 114(8):681-690.
- Szabo et al. 2015. Detection of hepatitis E virus RNA in raw sausages and liver sausages from retail in Germany using an optimized method. Int J Food Microbiol. 215:149-56.
- Tamada et al. 2004. Consumption of wild boar linked to cases of hepatitis E. J Hepatology. 40(5):869-870.
- Tei et al. 2004. Consumption of uncooked deer meat as a risk factor for hepatitis E virus infection: An age- and sex-matched case-control study. J Med Virol. 74(1):67-70.
- Teo et al. 2010. Much meat, much malady: changing perceptions of the epidemiology of hepatitis E. Clin Micro Inf. 16(1):24-32.
- Yugo. 2013. Hepatitis E Virus: Foodborne, Waterborne and Zoonotic Transmission. Int J Environ Res Pub Health. 10(10):4507-4533.