Leptospirosis
Etiology
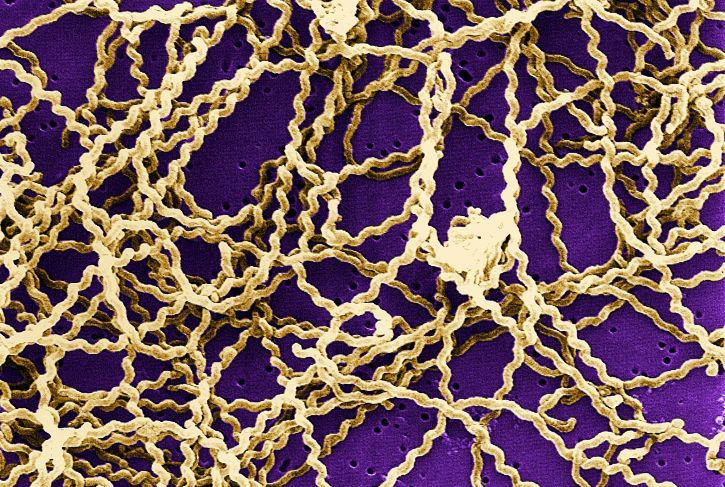
Leptospirosis is a disease caused by bacteria belonging to Leptospira genus. Leptospirae are Gram negative spirochetes, obligate aerobes, helical shaped, flagellated and mobile. This genus is composed of two species: Leptospira interrogans (which includes the pathogenic forms) and Leptospira biflexa (nonpathogenic or saprophytic forms). These species are divided into serogroups and serovars. L. interrogans contains more than 218 serovars organized into 23 serogroup.
Epidemiology
Leptospirosis is worldwide distributed, mainly in humid tropical and subtropical areas. The disease can affect domestic and wild mammals, reptiles, amphibians and humans. Horses are considered accidental hosts. The main source of infection is through the urine of infected, asymptomatic and carrier animals, usually small mammals such as rodents. Transmission can also be indirect through contaminated materials such as water, fodder, grass, saliva, semen, milk, vectors (flies, mosquitoes), postpartum tissues, etc. On the other hand, Leptospira can also be vertically transmitted (through the placenta) and venereally transmitted.
Pathogeny
Leptospira is introduced into the body mainly through the skin or mucous membranes and after the incubation period (4 to 10 days) it spreads through the bloodstream to different organs: liver, kidneys, lungs, cerebrospinal fluid, eye, mammary glands and reproductive tract (placenta). In the case of a pregnant animal, Leptospira invades the foetus, where they produce organic alterations similar to those in adults.
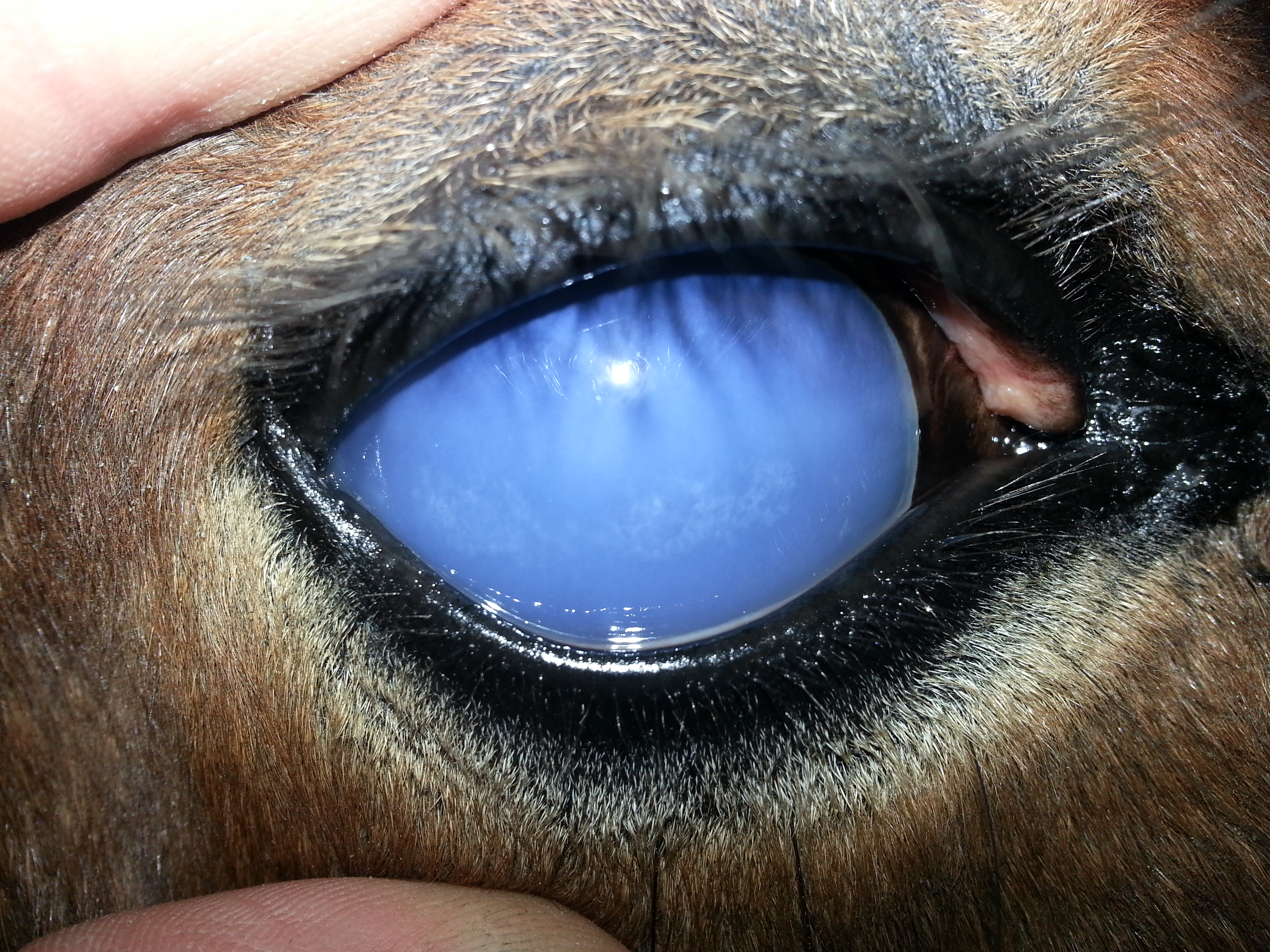
In horses, leptospirosis is usually associated with abortions and uveitis, although renal, hepatic and systemic failures may also occur. It is considered that abortion occurs due to systemic endothelial lesions, which also occur in the placentas and impede the transfer of nutrients and metabolites between the mother and the foetus. The uveitis or iridocyclitis of horses is caused by a type II hypersensitivity reaction, due to an antigenic relationship of Leptospira with the surface of the cornea and the lens.
Clinical signs
Initially in the majority of cases horses manifests nonspecific symptoms (anorexia, depression, fever, muscle weakness) and in some cases jaundice and petechiae in mucous membranes are present, in addition to hemolytic anemia.
Leptospirosis in pregnant mares can cause abortions (usually from the middle of gestation), premature births, stillbirths and the birth of nonviable foals. The placenta may appear thickened, edematous and hemorrhagic.
Horses with leptospirosis frequently develope uveitis, also known as periodic ophthalmia, recurrent uveitis or lunar blindness that is usually recurrent or persistent and may occur months to years after infection.
Systemic leptospirosis is not frequent in equids. When it occurs it can produce septicaemia accompanied by fever, weakness, anorexia, lethargy and jaundice and, occasionally, death. If the animal survives an infectious process occurs in the kidney. Hemoglobinuric nephrosis and anemia may occur when the hemolysis is severe.
Diagnosis
The diagnosis of leptospirosis depends on the combination of a good clinical history and specific and sensitive laboratory techniques.
Indirect methods (detection of antibodies against Leptospira) are the most frequent used to detect Leptospira, due to the difficulties that the direct detection of these pathogens presents. Antibodies detection is mainly performed by ELISA and MAT (microscopic agglutination test) techniques, in serum or other samples as aqueous humor.
The reference diagnostic test is MAT, in which the serum is confronted with an antigenic suspension of Leptospira.
Regarding to direct detection techniques, direct visualization in a microscope, culture of the microorganism, direct immunofluorescence and PCR, among others could be used. Samples of choice are urine, blood, cerebrospinal fluid, milk, tissues, etc.
To perform the culture it is necessary to have special culture media. Moreover, it is a not so sensitive and slow technique, so it has now been replaced by molecular techniques, which detect the microorganisms DNA, such as PCR, high sensitive and applicable to large number of samples.
Finally in the necropsy in the acute form of the disease it is common to find signs of anemia, jaundice, haemoglobinuria and submucosal and subserosal haemorrhages. Histologically, there is diffuse and focal interstitial nephritis, centrilobular hepatic necrosis and, in some cases, vascular lesions in the meninges and brain. The aborted foetuses and the placenta are oedematous and in an advanced state of autolysis or putrefaction.
Treatment
The treatment of leptospirosis depends on the location and severity of clinical signs and also if the animal is in an acute or chronic phase of the disease.
Some antimicrobials recommended in horses are dehydrostreptomycin, penicillin, sterptomycin, oxytetracycline and erythromycin. Occasionally, supportive therapy including fluid therapy and furosemide is administered.
In cases of uveitis, gentamicin is also recommended in addition to mydriatic and anti-inflammatory agents.
Prevention and control
The prevention and control of the disease are based on: management measures, vaccination and proper use of antibiotics.
The management measures are aimed at trying to eliminate any source of infection including limiting exposure to contaminated water, avoiding contact of susceptible animals with infected ones and with rodents, deratting, isolating infected animals, applying correct of hygiene and disinfection measures, etc.
Currently, there are no vaccines against leptospires authorized for use in horses although sometimes bacterins are used (bacteria killed by hit or formalin).
Public Health Considerations
Leptospira is a zoonotic bacteria, which can cause serious illness in humans, including death. The most frequent source of infection to humans is through direct or indirect contact with urine of infected animals, so the best way to prevent the disease is to avoid such contact. Population at risk: veterinarians, farmers, slaughterers, hunters, etc. must take extreme protection measures (gloves) and hygiene and disinfection measures.
References
- https://thehorse.com/126846/leptospirosis-what-is-it/
- https://www.sciencedirect.com/science/article/pii/S0378113513002150?via%3Dihub
- http://www.oie.int/fileadmin/Home/esp/Health_standards/tahm/2.01.12_Leptospirosis.pdf
- Equine Infectious Diseases. 2014 Elsevier Inc. ISBN: 978-1-4557-0891-8.