Surra
Etiology
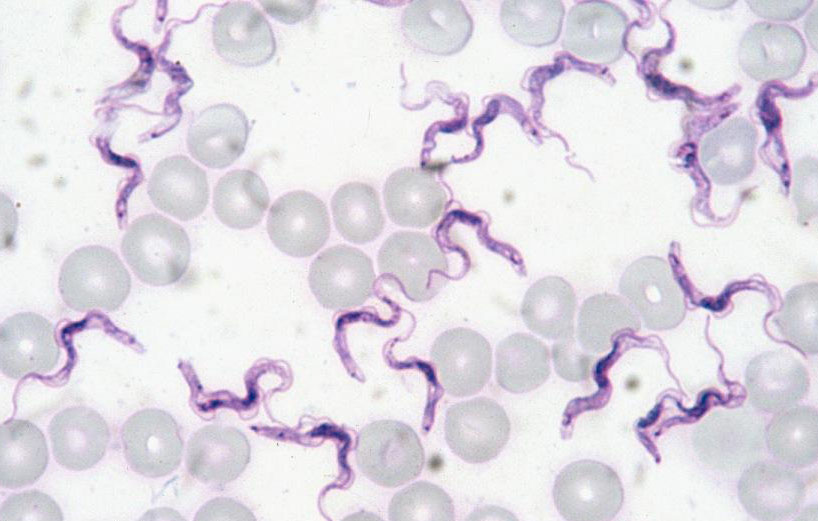
Surra is a disease caused by the flagellated protozoan Trypanosoma evansi. This parasite measures from 14 to 33 μm in length and from 1.5 to 4 μm in width and has a free flagellum and a subterminal kinetoplast.
Epidemiology
T. evansi has a very wide range of hosts, equids being one of the most commonly affected animals, especially in Central and South America. Surra has a worldwide distribution and causes great morbidity in Africa, Asia and South America. This parasite can be found in the blood and tissues of infected animals and carnivores can be infected by oral transmission. In horses it is transmitted mechanically by the bite or bite of a vector. The main vectors are hematophagous flies, mainly from the genus Tabanus. Ticks and vampires have also been described as vectors, with iatrogenic, venereal and milk transmission also possible. In equidae, the incubation period is from 5 to 60 days.
Pathogeny
Surra can be an acute, subacute or chronic disease. Some animals die quickly, especially in the case of free or susceptible animals that are transferred to endemic regions; in other cases, the clinical signs may persist for months and even the infection may be asymptomatic. T. evansi is multiplied by extracellular longitudinal binary fission in the blood, lymph and cerebrospinal fluid of the vertebrate host. This parasite has strategies to evade the immune system such as the presence of variable surface glycoproteins (VSG) or the production of constitutive and excreted/secreted factors that allow its survival. The infection usually occurs with lymphopenia, lymphadenopathy and splenomegaly. The pathogenesis of the infection varies according to the virulence of the strain, the susceptibility of the host, as well as concomitant non-specific factors such as stress.
Clinical signs
There are no pathognomonic signs or specific macroscopic lesions. Common clinical signs in the horse include fever (intermittent in chronic cases), weight loss or atrophy, lethargy, signs of anemia, dilation of the lymph nodes and spleen, as well as postural edema. Urticaria, jaundice and petechial hemorrhages are also observed in mucous membranes. Neurological signs, in the final stages of the disease, are ataxia, with gradually progressive paresis of the hindquarters, accompanied by muscular atrophy. Other signs may also appear, such as head tilted, circular movements, hyperexcitability, blindness, proprioceptive deficit and rowing movements. Infertility, abortions and / or stillbirths have been recorded. T. evansi causes leukopenia, which can generate immunosuppression.
Diagnosis
The differential diagnosis must include African horse sickness, equine viral arteritis, equine infectious anaemia, equine babesiosis and other chronic parasitism. In horses with encephalitis, equine myeloencephalopathy due to herpesvirus type 1, western, eastern or Venezuelan encephalitis, protozoan equine myeloencephalitis, West Nile virus infection and rabies should be considered. The recommended laboratory methods for diagnosis are 1) Microscopic examination of a Giemsa-stained thin blood smear from the host, or from a mouse inoculation test, allows identification of the subgenus Trypanozoon based on morphology and morphometry of parasites. 2) PCR-TBR: DNA must be prepared from blood with using the buffy coat. 3) ELISA T. evansi: Serum or plasma samples are tested. 4) CATT for T. evansi: Serum or plasma are diluted 1:4. Positive samples are samples presenting results = or > to one + (doubtful samples are considered as negative samples).
Treatment
In endemic areas, antiparasitic agents are used. Highlights include suramin, diminazene, melarsomine and quinapyramine. No vaccines are available for this disease.
Prevention and control
Early detection prevents the disease from becoming enzootic in free regions. Eradication is achieved through quarantine measures, movement control, isolation and slaughter of infected animals. It is also important to control arthropod vectors and the confinement of healthy animals during daylight hours. In endemic areas, surra is usually controlled by treating infected animals and controlling the occurrence of resistance and toxic effects of antiparasitic agents.
Public Health Considerations
T. evansi is a non-zoonosic triponosome, although human infection is documented in congenital disorders of resistance apolipoprotein to animal trypanosomoses. Surra is a disease included in the OIE list of notifiable diseases.
References
- OIE Terrestrial Animal Health Code
- OIE Manual of Diagnostic Tests and Vaccines for Terrestrial Animals
- IAState Center for Food Security & Public Health Factsheets