West Nile Fever
Etiology
WN virus belongs to family Flaviviridae. Some other members are: virus of Japanese encephalitis, dengue, St. Louis encephalitis and yellow fever. There are two lineages based on differences between outbreaks onsets in different areas. Lineage I is present in Africa, India and Australia, and is responsible for the outbreaks in Europe and the Mediterranean area. A variety of this lineage is responsible for the deaths of thousands of wild birds and geese in Israel in 1998, as well as for the outbreak of New York in 1999 and its subsequent spread in the United States. Lineage II is only evident in sub-Saharan Africa. It is an arbovirus (arthropod-borne viruses).
Epidemiology
WNV is an arbovirus (arthropod-borne viruses) transmitted through the salivary glands of mosquitoes of different genres, mainly generi Culex and Aedes. In Europe, three are the main vectors: Culex pipiens, Culex modestus and Coquillettidia richiardii. Many avian species can become infected, but family Corvidae, (crows, magpies...) are the most susceptible to disease. Corvidae tend not to overcome the disease and die. For that reason they are used as sentinel animals.
Infected birds develop a strong viremia, allowing another mosquito to capture the virus when feeding and allowing transmission within an ornithic cycle. Some amphibians (Rana ridibunda) also develop a high viremia, but its epidemiological role seems limited. Mammals are accidental targets for these mosquitoes, and terminal hosts in terms of epidemiology. Biological cycle will end in them as they develop an insufficiently intense viremia to enable another vector to acquire the virus. Both antibodies and WN virus have been detected or isolated in many domestic and wild animals (squirrels, mice, camels, hares, skunks, bats, wolves, rabbits, dogs, cats... etc.), demonstrating viral circulation and contact with the virus. These accidental hosts seem not to contribute significantly to the transfer of the virus. On the other side, man (zoonosis) and horses, are the most susceptible species, developing the disease.
The increase in the circulation of the virus is favored by abiotic factors - heavy rains, flooding, rising of global temperatures - and biotic - increased populations of mosquitoes and birds (migratory or not) -, as well as by the influence of anthropogenic factors such as new settlements, travel, trade relations, intensive irrigation or open avian farms.
Pathogeny
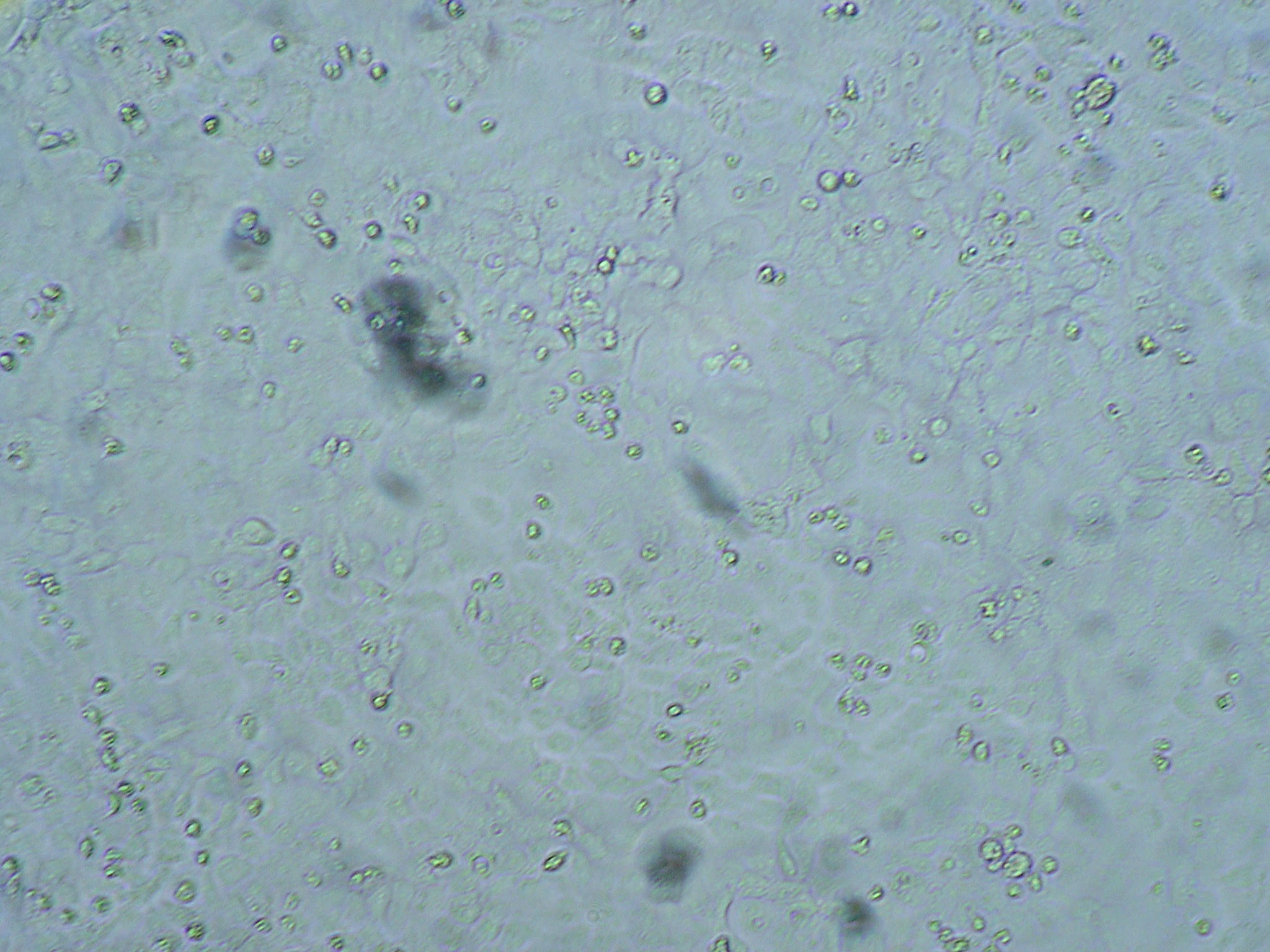
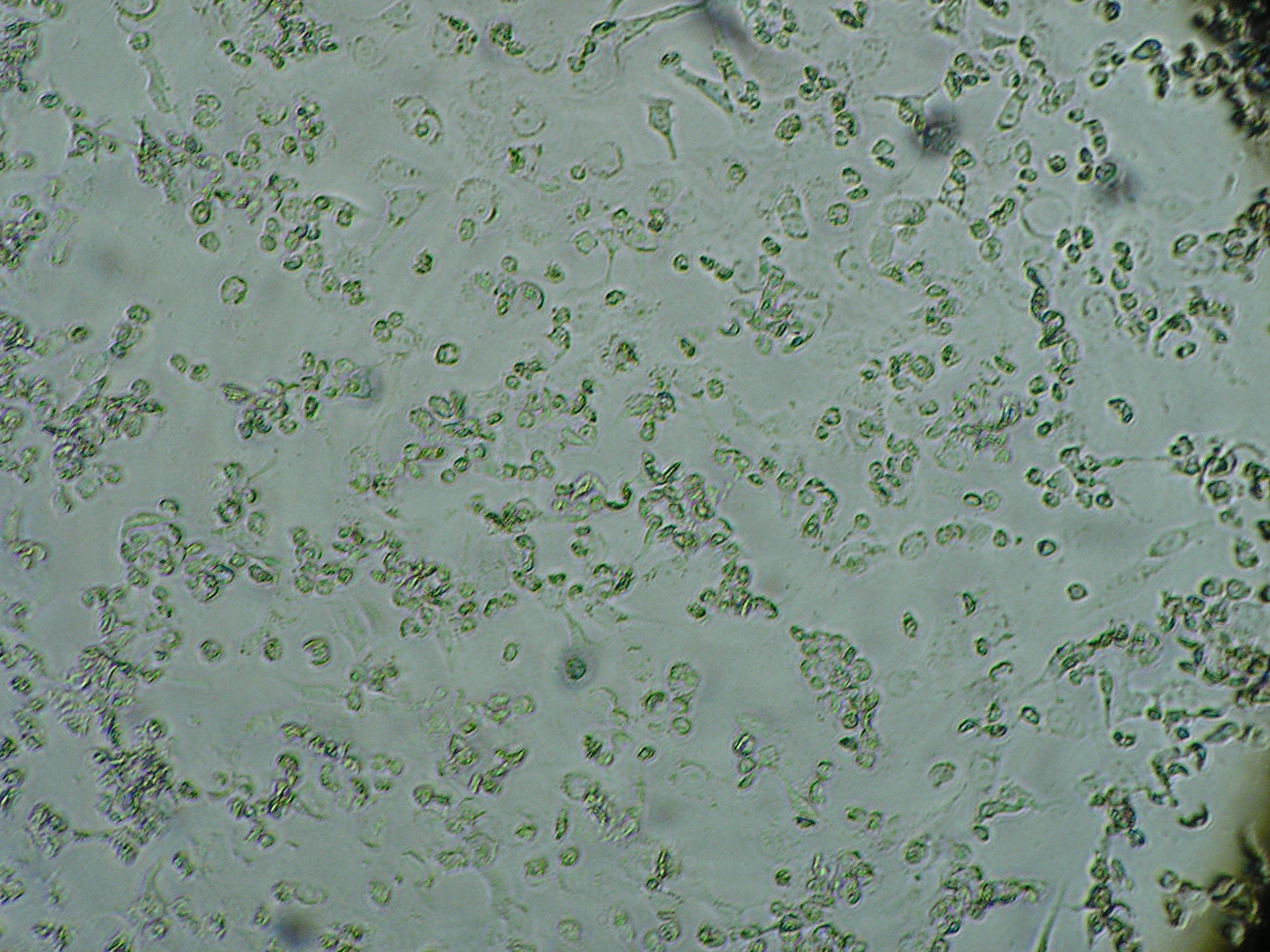
The acquisition takes place by the bite of blood-sucking mosquitoes. Having overcome the skin barrier, the virus reaches lymph or blood and spreads quickly. After multiplying in the cells of the vascular endothelium, reticuloendothelial cells of lymph nodes, fibroblasts and Langerhans cells, reaches target organs. Passive transfer or replication in endothelial cells of the vascular endothelium of Central Nervous System (CNS) is the main colonization mechanism, although there is a minor route by means of axonal transport through olfactory neurons. Once inside the CNS, virus spreads between cells by contiguity, with pathological changes including meningitis and encephalitis, edema, neuronal degeneration (vacuolization), gliosis, focal lesions in the previous antler of spinal cord and perivascular inflammatory infiltrates of mononuclear cells.
Clinical signs
Both in man and horse, the majority of infected individuals remain asymptomatic. If they develop clinical signs, these are both systemic and neurological. There is fever, anorexia and stillness, which often follow in abdominal pain (sometimes colic in horses). The most obvious signs ruling the clinical diagnosis, are abnormalities in gait. In horses (but also in man) appears, typically, a slow and short gait (bradykinesia), sometimes with overt lameness, to the point of dragging one limb. Evolution tends to progress with purely nervous signs, both spinal and central. The first they may include ataxia and flaccid paresis. Central nervous signs include fasciculation of facial and cervical muscle groups and alterations in behavior, with periods of hyperexcitability (including photophobia and aggressiveness) or depression.
Diagnosis
Differential diagnoses should include alphavirus encephalitis, rabies, equine protozoal myeloencephalitis, equine herpesvirus type 1, botulism, and parasitic meningoencephalomyelitis (e.g., Halicephalobus gingivalis, Strongylus vulgaris).
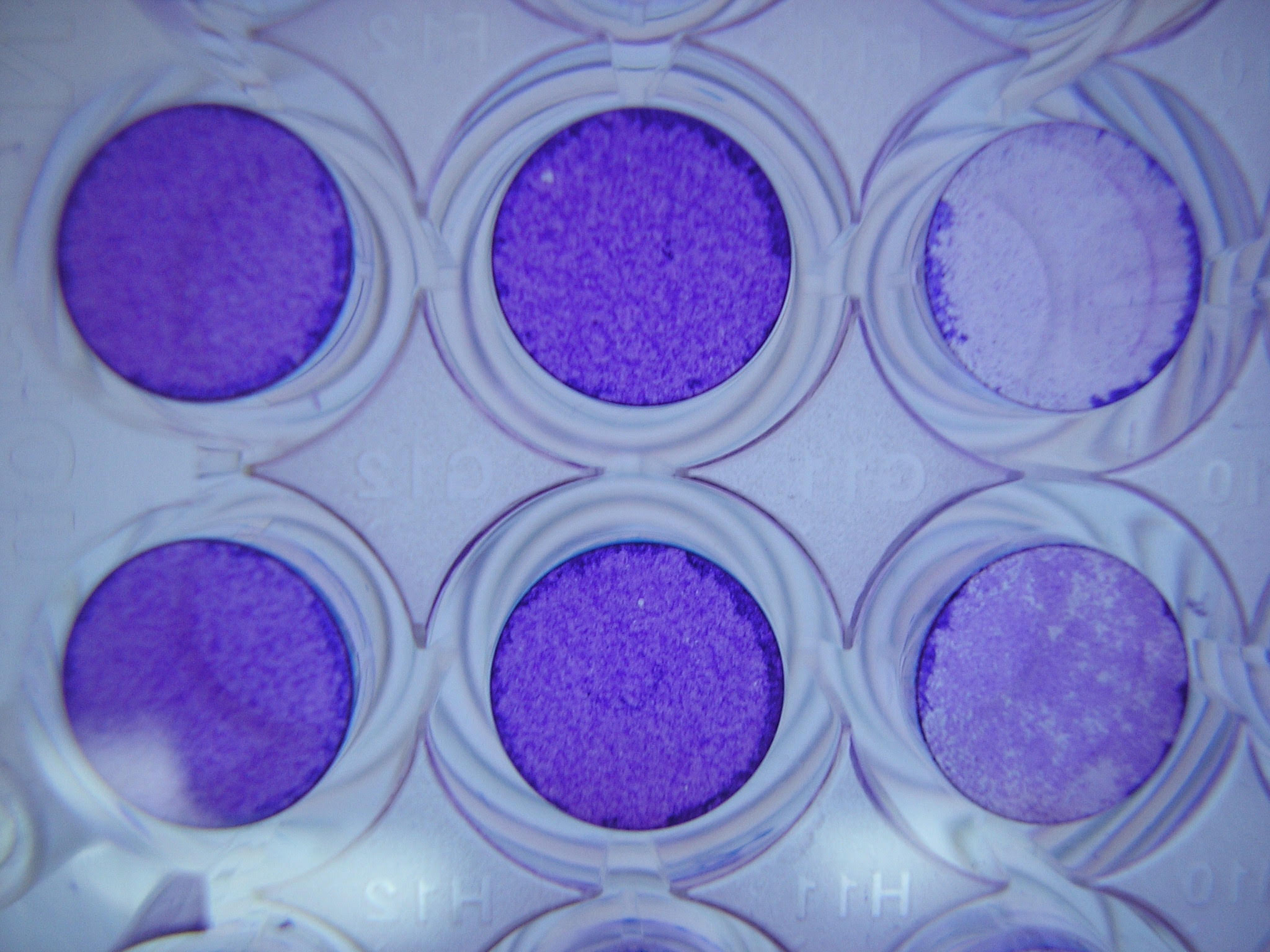
Based on clinical and epidemiological evidences (signs, presence of mosquitoes, season, previous events etc.), laboratory tests may include serological tests or antigen detection. The first, include the detection of IgMs, occurring steadily in acute infections and can last up to 6 weeks in horses, unlike the response in humans, much less evident. Most used and reliable is the capture ELISA (MAC-ELISA) and positive seroconversion, valid in any species and therefore useful in serological surveys. Also available for horses is an indirect ELISA system (IgM and IgG), differential ELISA among WNV and other flavivirus, based on detection of antibodies against non-structural proteins. Last, an ELISA-DIVA system is available that discriminate vaccinated from infected animals. The detection of antigens can be done using RT-PCR techniques, allowing differential detection of lineages I and II.
Treatment
There are no specific antiviral treatments for infection by West Nile virus. While analgesics can be used to reduce fever and relieve some symptoms, in more severe cases, patients are usually hospitalized to receive symptomatic treatment and monitoring.
Prevention and control
Surveillance should focus on mosquitoes, birds and horses. Major interest areas, but not solely, are those close to wetlands. Control of WNV must include actions on each element of the cycle: vector, main host (birds) and accidental host (mammal). This implies an active surveillance on birds to detect mass (or unusual) mortalities among wild populations, this making them serve as sentinels for the presence of the virus. Together, an active surveillance on vector mosquito and the identification of other potential vectors in a specific area should be addressed by means of a preventive program of integrated control of mosquito populations based on physical, chemical, biological, and educational fight methods.
Public Health Considerations
The passive surveillance in animals and people is important. This should enhance the declaration of neurological diseases in animals, especially birds and horses, reservoirs which, by its potential relationship with man, can transmit the disease. In humans, cases of aseptic meningitis and encephalitis without etiological diagnosis should be notifiable.
References
- Asamblea mundial de delegados de la OIE. (2013). Fiebre del Nilo Occidental. Manual terrestres de la OIE, capítulo 2.1.24.
- Chimeno Risco, Pedro, et al. (2017). West Nile Virus en caballos. Badajoz Veterinaria (Revista del colegio oficial de veterinarios de Badajoz), 8: 6-12.
- Donadieu, Emilie, et al. (2013). Differential Virulence and Pathogenesis of West Nile Viruses. Viruses, 5: 2856-2880.
- FAO. West Nile Disease. World situation and impact on public health.
- FAO-OIE-WHO Joint Scientific Consultation. (2010). Influenza and other emerging infectious diseases at the human animal interface.
- García-Bocanegra, I. et al. (2017). Epidemiology and spatio-temporal analysis of West Nile Virus in horses in Spain between 2010 and 2016. WILEY: Transboundary and empirical diseases, Facultad de Veterinaria de la Universidad de Córdoba.
- Groen, T.A. et al. (2017). Ecology of West Nile virus across four European countries: empirical modelling of the Culex pipiens abundance dynamics as a function of weather. BMC (Parasites & Vectors), 10: 524.
- M. A. Jiménez – Clavero, F. Llorente, E. Sotelo, R. Soriguer, G. Gómez – Tejero, J. Figuerola (2010). West Nile Virus serosurveillance in horses in Doñana, Spain, 2005 to 2008. [en línea] PubMed [Fecha consulta: 17-02-2018].
- Ministerio de Medio Ambiente, Medio Rural y Marino (MAPAMA). Enfermedad Fiebre del Nilo Occidental (West Nile).
- Pérez, E. J. P. (1992). Enfermedades infecciosas y microbiología clínica.
- Rizzoli, Annapaola, et al. (2015). Understanding West Nile virus in Europe: Culex pipiens host feeding preference in a hotspot of virus emergence. Parasites & Vectors, 8: 213.
- Sambri, V. et al. 2013. West Nile virus in Europe: emergence, epidemiology, diagnoses, treatment, and prevention. University of Bologna. Clinical Microbiology and Infection, 19: 699-704.
- World Organisation for Animal Health (OIE). Fiebre del Nilo Occidental.
- Zoetis, España. West Nile Virus.